We know a few things for sure about SARS-CoV-2, the virus that causes COVID-19: It had likely been hiding in animals for decades prior to the current human pandemic, the course of the disease and the prognosis vary widely among individuals, and it’s incredibly difficult to destroy. “Coronaviruses are one of the few RNA viruses with a genomic proofreading mechanism, which keeps the virus from accumulating mutations that could weaken it,” explains David Cyranoski in a Nature news feature. “That ability might be why common antivirals such as ribavirin, which can thwart viruses such as hepatitis C, have failed to subdue SARS-CoV-2.”
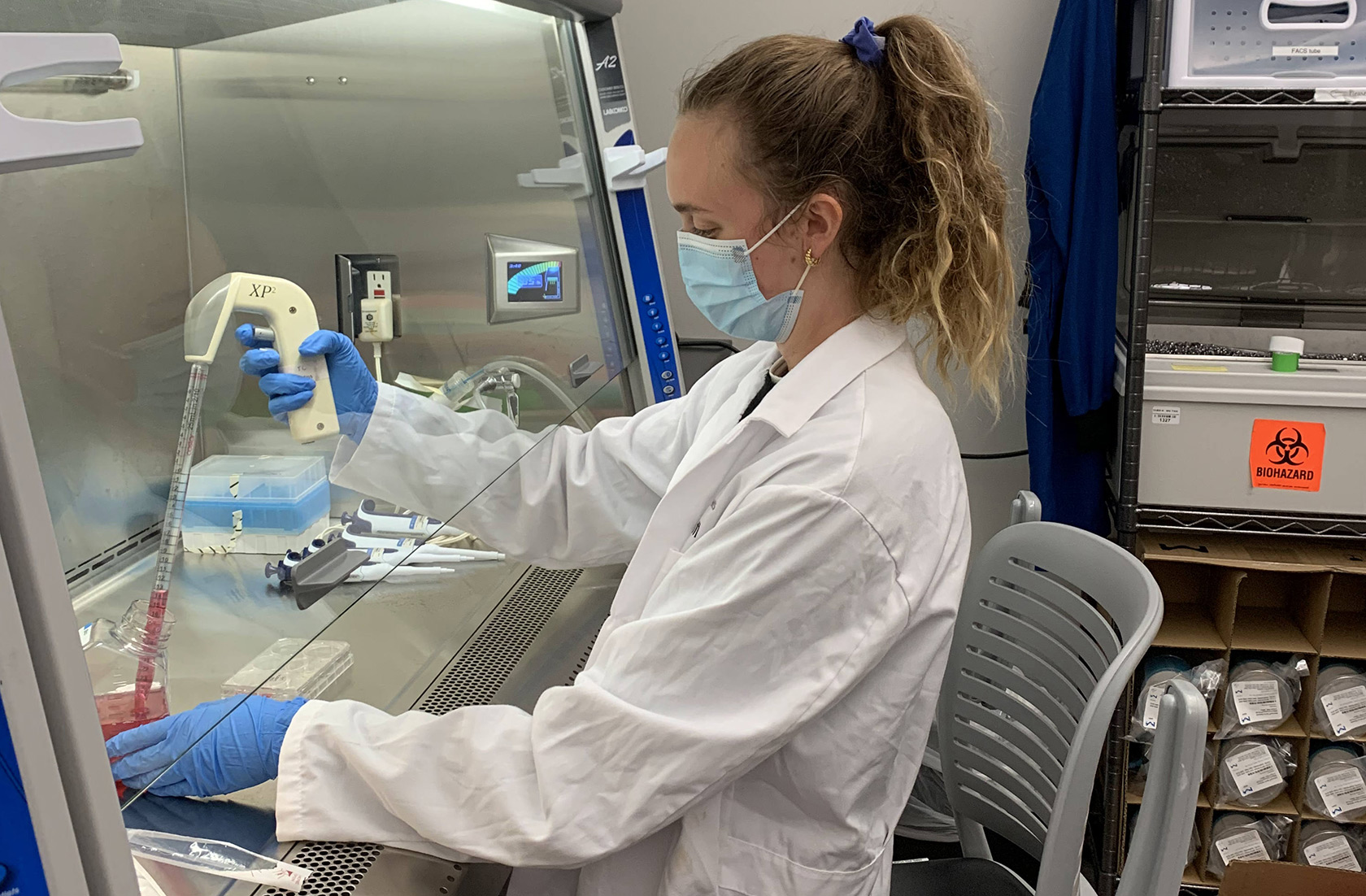
But researchers in the lab of Stanley Qi at Stanford University, where Laine Goudy ’18 works as a life science research professional, have solved a piece of the puzzle by using CRISPR gene-editing technology to fight the coronavirus. In an approach the lab called PAC-MAN (Prophylactic Antiviral CRISPR in huMAN cells), the researchers directed CRISPR to attack the part of the virus’s genetic makeup that enables it to penetrate and replicate within human cells.
“Think of CRISPR as molecular scissors—it’s a two-part process involving an enzyme that acts as the scissors and a guide RNA that acts as a kind of homing molecule, telling the enzyme where to cut,” explains Goudy.
Prior to the COVID-19 pandemic, the Qi Lab, known for their expertise in genetic engineering and synthetic biology, was already developing CRISPR tools to help cells become their own weapons against disease. The lab was utilizing this technology to create a universal influenza vaccine under a Defense Advanced Research Projects Agency (DARPA) grant when they first heard about the novel coronavirus. As both influenza and COVID-19 are RNA viruses, “they were similar enough that we could just tweak our platform to be able to target the coronavirus,” Goudy says.
Just a few short months later and the team’s results have been published in the peer-reviewed journal Cell, where Goudy is a co-first author. The team found PAC-MAN could reduce the amount of virus in vitro by 90 percent. “We theorized that with an effective delivery mechanism, this approach might be able to stop the disease within a human.”
Because so few labs have the biosafety level certification to work with actual strains of SARS-CoV-2, the Qi lab developed a synthetic strain to test their CRISPR platform. Now, they are partnering with a lab run by Sarah Stanley at the University of California, Berkeley that has the biosafety certification to test the platform with the live virus.
Back at Stanford, Goudy is wrapping up her responsibilities as she prepares to start graduate school in the fall. “I wanted to gain more hands-on lab experience before applying to graduate school,” she says. While in the Qi lab, she has conducted experiments, presented a poster at a conference, and is now an author on two published papers. The experience has paid off: This fall, she will begin a PhD program in biomedical sciences at the University of California, San Francisco.
“I was always really interested in science, taking AP biology in high school, and I really clicked with the subject and was fascinated by biological systems—it’s not just basic biology I wanted to learn more about, but also how it’s applied to human disease,” she says. A biochemistry major at Scripps, Goudy spent a year working in Professor Larry Grill’s lab, which focuses on vaccine development. “That got me really thinking about the host-pathogen interface for the first time. It was definitely formative – it was my first experience working in a lab, thinking about the innate immune system, infectious disease, and how can we better protect humans from viral pathogens,” she recalls. The summer after her junior year, she also participated in the Summer Undergraduate Research Program (SURP) at the Fred Hutchinson Cancer Research Center, where she learned about small molecule drug therapies for Hodgkin’s Lymphoma.
“It’s just so exciting to be working in a space so applied and relevant to today’s current events,” Goudy says. “I think that the fields of CRISPR and cell engineering have so much room to grow within the next five years—they have the potential to revolutionize how we think about conventional pharmaceuticals.”

